Monday to Friday, 7 AM – 7 PM CST.
If you're reaching out outside these hours, please submit a support ticket—our team will respond as soon as possible.

ABA Session Notes: Components, Examples, Templates and Expert Tips
Documenting patient progress is fundamental to ABA. Learn how to write session notes, explore examples, and download free templates. Get expert tips on how to write effective notes that will meet both clinical and insurance needs.
Inside this article:
- The differences between ABA session notes and ABA SOAP notes
- The main components of ABA session notes
- How to meet ABA session note insurance requirements
- Expert tips for writing ABA session notes
- How to use technology to help write ABA session notes
What are ABA Session Notes?
ABA session notes are detailed forms describing what happened during an ABA therapy session. The provider writes the notes with basic patient information and a narrative summary of the treatment. The notes also describe behavior targets, intervention types, and data.
Also, session notes are key for insurance claims validation. Payors request session notes to confirm that the provider performed the services on a claim and that the intervention was medically necessary and relevant. The bottom line is that payors look to session notes to help substantiate the medical need for ABA treatments.
In a 2021 paper published in the Journal of Behavioral Analysis, the authors discuss how higher demand for ABA services has increased the number of insurance companies covering behavior analysis services.
The authors write, “The increase in funding by insurance companies is paired with an increase in documentation requirements that can serve as a record of a billed session, substantiate the need for therapy, outline response to treatment, document coordination of care, and note other pertinent events. Session notes are one example of clinical documentation commonly required by insurance companies.”
The paper, titled “The Use of a Brief Treatment Package to Increase Session Note Completion in an ABA Agency,” observes that session notes lack a common standard despite their importance.
The authors go on to describe how session note templates and checklists could help ABA professionals take comprehensive session notes that meet payor guidelines.
Overall, session notes are incredibly important for both clinical and compliance reasons. As demand for ABA continues to grow, there is a growing recognition that the field will benefit from standardized session notes that fulfill all payor requirements and capture all the important clinical information that other medical and behavioral professionals might need. Understanding how to read and write these notes is essential for ABA practitioners.
Key Takeaways:
- Session notes are the primary form of medical documentation in ABA.
- All insurance payors require that you submit session notes as part of a pre-payment audit.
- Session notes contain only objective data, unlike SOAP notes, which also have subjective observations.
- Clinicians use session notes to track patients' progress and tailor their treatment.
- The best practice management software includes session note templates that help ABA clinicians fulfill payor requirements.
ABA Session Notes Vs. ABA SOAP Notes
ABA session notes differ from SOAP notes in both their content and approach. SOAP notes include both subjective and objective insights and recommendations. Meanwhile, session notes objectively focus on the session’s treatment, goals, and results. Both are essential client records in ABA.
SOAP notes are a standardized method for recording clinical sessions that many medical professionals use. The acronym “SOAP” delineates the four key sections of these notes: Subjective, Objective, Assessment, and Plan. In the context of ABA, both SOAP notes and session notes play an important role in comprehensive client records. However, they fulfill distinct roles and document different facets of a therapy session.
“In BCBA, we use SOAP notes and session notes to target different goals,” explains Torres. “Most use SOAP notes when they’re meeting regularly with a patient to target a very specific issue. These notes blend subjective client observations and objective information and include recommendations for future interventions to help the patient progress on their specific goal. BCBAs and their colleagues usually read these narrative notes to understand session nuances and plan future goals."
Torres continues, "On the other hand, session notes contain objective descriptions about what happened during the session. They're accessible to a broader audience, ranging from insurance payors to the child's teacher. The focus is on what happened in the session and doesn’t include information on subjective recommendations or opinions from the BCBA or RBT."
Torres illustrates one key difference between session notes and SOAP notes with an example: "In a SOAP note, you might start with subjective observations that the ABA practitioner writing the notes feels is relevant, such as 'The patient seemed happy.' However, this type of opinion-based language is not suitable for a session note. Instead, a session note would clearly identify the goal and summarize intervention data, like 'The client smiled and laughed when he greeted the therapist. The client was given ten opportunities to execute a target and responded correctly 70% of the time.’ "
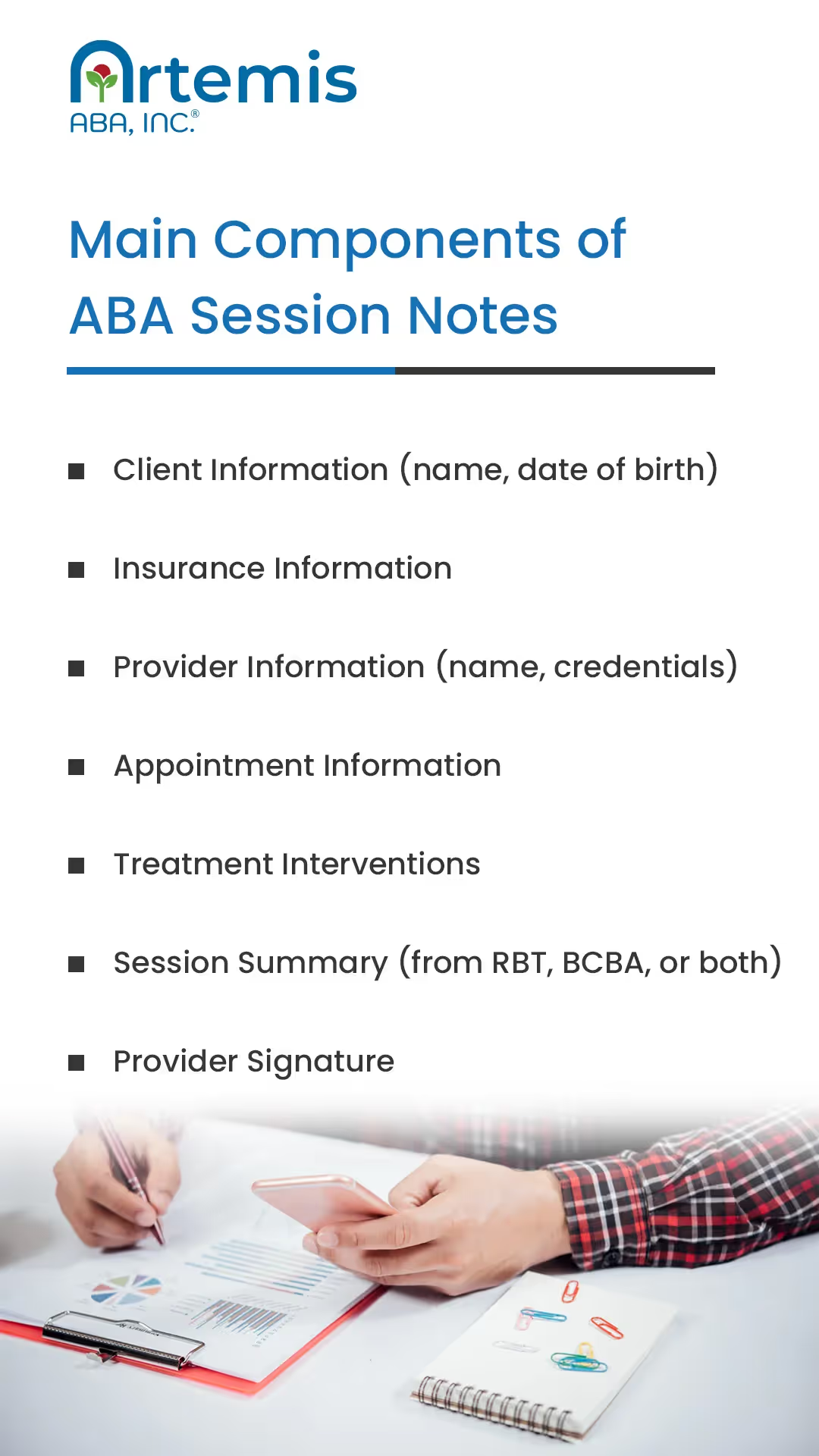
Main Components of ABA Session Notes
The main components of ABA session notes include basic details about the client, the provider, and the session. The core of these notes is a narrative summary. This part outlines interventions, data, and other information that explains what happened during the session.
ABA session notes contain clinical and non-clinical components. While requirements vary among insurance providers, clinical categories typically include a basic summary and detailed descriptions of interventions. Alongside these clinical details, most insurers require basic information like the client’s name, the appointment date, the length of the session, and data about the provider and any other session participants.
Here’s a summary of the main categories of ABA session notes, with examples. This list includes all the requirements from most major ABA insurance payors. However, it's important to note that this list is not exhaustive, as payors may have different requirements that are subject to change.
Client Information
Appointment Details
Provider Information
Treatment and Session Details
These sections describe the specific events of the session and end in a narrative summary that the rendering provider writes.
Why ABA Session Notes Are Important
Session notes are important for many reasons. They substantiate billing claims and justify the need for services from payors. They’re crucial for BCBAs to document and monitor the patient’s progress. Session notes help ABA professionals communicate with others, like doctors and teachers.
Taking notes is critical in all medical professions, and ABA is no exception. These notes represent the provider’s summary of what happened during the session, how that relates to the patient’s ongoing progress, and what might happen next. The notes are the only way to document and track the patient’s progress accurately. They’re of interest to anyone involved in the patient’s care—including parents, other medical professionals, and insurance payors.
Here’s a summary of the main reasons why ABA session notes are important:
ABA Session Notes Insurance Requirements
Most insurance payors don’t require session notes to make a claim. When payors audit claims, they require session notes to prove that the provider performed a service. Session note requirements vary, but most payors require details about the patient, provider, and specific interventions.
Payors request session notes whenever they decide to audit a claim. The session notes should support that the clinician performed the services on the claim and that the treatment was medically relevant. Although you don’t need session notes to submit a claim, they’re incredibly important to pass these inevitable audits. Insurance payors have similar session note requirements, although sometimes minor differences exist.
Specifically, session notes come into play whenever a payor wants to conduct a pre-payment review (PPR) audit on your claim. During a PPR, payors are looking for clear documentation that lines up with the information on the initial claim. “
Khan says it’s not “if” you’ll get a PPR audit but “when.”
“You won’t be able to pass an audit if you don’t have complete documentation that proves that you provided the services you are claiming, and that these services were necessary for the patient. If you’re not in the habit of keeping high-quality session notes, a payor will probably find something in your notes that doesn’t meet their documentation requirement, and they’ll deny your claim, which amounts to money lost.”
Khan emphasizes that you won’t know which dates of services a payor will select to audit. “The best way to approach these audits is to set up a solid documentation system that meets payor requirements,” he says. “Then, you know that if you receive an audit, you’ll have high-quality session notes to back up your claims.”
Khan underscores that different payors have different requirements, and it’s important to make sure you review these requirements with your major payors. He adds that all insurance providers want to see certain fields, so having them will help you pass any PPR audit. Khan says the key is to make it easy for the payor to see that you rendered the services you list on your claim. To do so, you must go beyond just summarizing your services in a few sentences.
“BCBAs and RBTs are busy. Most of them document every session, but everyone does it a little differently. Some do it immediately; others wait. Some focus on certain aspects of care, and others find something else, like data, more important. This variability means that, in the eyes of payors, most session notes aren’t very well-organized or easy to understand. In this case, even if you’re rendering the service correctly and faithfully, the payor might not see that reality reflected in your note.”
Khan continues: “To avoid this situation, it’s important to have templates with pre-defined fields for every piece of information that a payor requires. For example, the templates have a drop-down menu listing all the interventions that the provider can select from. There’s a space for the provider’s name, the client’s name, and more. Of course, the templates contain a blank field for a session summary. Using these templates simplifies the process for both insurance companies and healthcare providers: It’s easier for the payors to read quickly, and it’s much faster for the provider to write. Plus, they give the provider the assurance they need. If an audit does happen, they have nothing to worry about because they know that their session notes are comprehensive by default.”
Our free ABA session note template below includes all the categories that Khan and other experts say must be in every session note.
Expert Tips for Writing Effective ABA Session Notes
To write ABA session notes like an expert, follow some key tips: If possible, take notes immediately after the session. Use a template with pre-determined categories to fulfill all insurance requirements. Also, experts recommend writing notes on a computer with practice management software.
Here are more tips from clinical and insurance experts on writing ABA session notes that meet clinical and insurance needs.
Common Mistakes to Avoid in ABA Session Notes
All clinicians occasionally make mistakes in their session notes due to human error. One common mistake is using subjective language. Another is forgetting to list all the interventions they used.
Here's a list of the most common mistakes in ABA session notes:
Using Technology to Assist with ABA Session Notes
Using tech in ABA therapy makes it easier for therapists to write and keep track of their notes. They can use digital tools to write notes quickly, add information immediately, make changes, and keep notes safe and secure. This software ensures that session notes are organized, accurate, and easily accessible.
“Taking session notes with an ABA Practice management software saves you so much time, helps you take more compliant notes, and takes away the stress of storing the notes somewhere safe,” Torres says. "This specialized ABA software has really helped BCBAs and RBTs shift their focus to what truly matters: meaningful client interaction, rather than getting bogged down in note management and paperwork.”
Here's a list of why ABA practice management software tech helps improve ABA session notes:
Using ABA Practice Management Software for Session Notes
ABA practice management software includes session note templates that help clinicians take comprehensive notes. Artemis’ end-to-end software offers a holistic ABA solution with session notes, data collection, billing and more.
Artemis ABA stands as the industry leader in ABA practice management software. It employs advanced technologies like AI and machine learning algorithms to help ABA clinics optimize their practices and deliver superior care.
Artemis integrates session notes as a critical part of its comprehensive ABA practice management solution. It offers tailored templates for RBTs and BCBAs, ensuring compliance with PPR audits and enabling clinics to maintain thorough, comprehensive records that fulfill clinical and insurance needs. These templates are user-friendly, detailed, and accessible from anywhere. Plus, clinicians can easily switch between multiple active sessions to take notes on many patients at once.
Along with session notes, Artemis' end-to-end software integrates data collection, reporting, scheduling, billing, and more within its single, unified platform. You can efficiently switch between multiple active sessions for notetaking. Each patient's profile includes a dashboard with tools for data collection, scheduling, and behavior intervention plans. Additionally, advanced reporting and analytical tools enable you to understand whether your plan is working and develop personalized, data-driven approaches for each patient.
Artemis ABA is the unparalleled choice for clinics seeking to fully digitalize their ABA practice and enhance patient care.
Schedule Your Walkthrough
Please enter your details and one of our team members will contact you shortly
See Artemis in Action
Enter your information below












%201.webp)


